Clinical highlights – July 2022
We are thrilled to inform you about the science of eye tracking. Every month, we will keep you updated on the latest news shared by the scientific community. The newsletter of this month is related to the analysis of eye movements for differential diagnosis of Multiple System Atrophy.
We are also excited to announce you that a first prototype of NeuroClues TM is ready! NeuroClues* is a portable lab that will help you instantaneously measure your clinical exam. Do not hesitate to contact us for a demo.
The P3Lab team
*The product is not yet available for sale and will soon undergo clinical investigations.
Multi System Atrophy (MSA) diagnostics challenges
Multiple system atrophy (MSA) is a progressive neurodegenerative disorder characterized by a combination of symptoms that affect both the autonomic nervous system and movement. The symptoms reflect the progressive loss of function and death of the different types of nerves cells in the brain and spinal cord. MSA is a rare disease with an annual rate of 0.1-3 per 100 000 depending on age and geographic region.
A distinguishing features of MSA is the accumulation of the protein alpha-synuclein in glia, similar in Parkinson’s disease, but in nerve cells. Making a diagnosis of MSA can be difficult, particularly in the early stages, in part because many of the signs are similar to those observed in Parkinson’s disease. Today, DaTscan can assess the dopamine transporter in the striatum and can help physicians determine if the condition is caused by a dopamine system disorder. However this test cannot differentiate between MSA and Parkinson’s disease.
The last two decades have laid the basis of the active search for MSA disease-modifying therapies. Significant knowledge has been generated on understanding the disease mechanisms, which made it possible to identify alpha-synuclein pathology and glial responses as significant targets to modulate the progression of the neurodegenerative process.
Therefore finding the right biomarkers and having the tool to differentiate at early stage MSA from Parkinson’s disease would greatly accelerate clinical research by improving patient selection, shortening the timeframe needed to show that a drug has successfully engaged a disease-specific target in the brain or nervous system. Biomarkers may also be useful for determining optimal drug dosage.
Source: NIH
Eye tracking, a quest for objective biomarkers in differentiating MSA from PD
There is a wealth of scientific knowledge about eye movements analysis for the differential diagnosis of MSA. We list here a few examples:
Expected variations of oculomotor biomarkers for pathological populations with movement disorders can help differentiate MSA from another movement disorder disease.
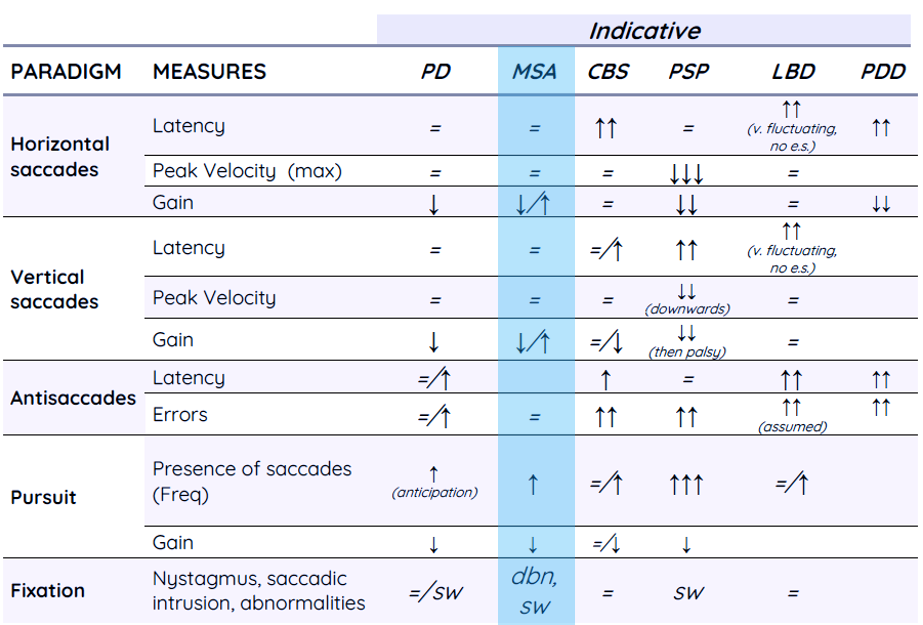
Légende: PD: Idiopathic Parkinson’s Disease ; MSA: Multiple System Atrophy ; CBS: Corticobasal Syndrome; PSP: Progressive Supranuclear Palsy ; LBD: Lewy body Dementia; PDD: Parkinson’s Disease Dementia; ATD: Alzheimer’s type Dementia; PNFA: Progressive Nonfluent Aphasia; FTD/tau: Frontotemporal Dementia – tauopathies ; FTD/TDP: Frontotemporal Dementia: – Proteinopathies; sw : square waves ; dbn : downbeat nystagmus ; e.s. : express saccade
Adapté de Leigh, R. &. Zee (2015-06). The Neurology of Eye Movements. Oxford, UK: Oxford University Press.
From December 2019 to January 2021, 30 patients with PD and 23 patients with MSA (17 with cerebellar-type MSA and 6 with parkinsonian-type MSA) had a video-oculographic recording of HITs at two university hospitals in South Korea. Researchers found that reversed (p = 0.034) and perverted (p = 0.015) catch-up saccades were more frequently observed in MSA than in PD during HITs.
Catch-up saccades are more frequently associated with MSA than with PD
Saccades in MSAP are characterized both by prolonged acceleration and deceleration periodes with reduced peak velocity. In contrast, the velocity profile of PD patients was characterized mainly by prolonged deceleration period
According to recent findings, saccade profiles provide useful information for differentiating between PD and MSAP at early stages. While the changes in velocity profiles may be explained by the cerebellar and brainstem pathology in MSAP, the changes in velocity profile in both PD and MSAP correlated significantly with increasing severity of Parkinsonism in both disorders, suggesting a link with striatonigral pathology.
Inspection of the saccadic component of pursuit tracking revealed that in MSA saccades typically correct for position errors accumulated during SPEM epochs (“catch-up saccades”), whereas in PD, saccades were often directed toward future target positions (“anticipatory saccades”).
The differences in pursuit tracking between PD and MSA were large enough to warrant their use as ancillary diagnostic criteria for the distinction between these disorder
You want to know more?
Our experts have gathered a comprehensive list of scientific literature about the analysis of eye movements for the differential diagnosis of Multiple System Atrophy. Feel free to contact us a request a copy
Did you miss our symposium in Paris last month?
Don’t worry, we recorded the presentations. Request your links here.